CMS – New Required Consents – English
CMS Requirement – Situation 1 (Not a Referral) and 2(Referral)
In June 18, 2023, two new requirements were established by the Department of Health and Human Services (HHS) and the Centers for Medicare and Medicaid Services (CMS) will come into effect.
Form 1: New consumer consent requirements:
Agents must obtain and document consumer consent before assisting or facilitating enrollment for coverage through federally facilitated exchanges and state exchanges on the federal platform or helping an individual apply for an advance premium tax credit or a cost-sharing reduction.
This consumer consent requires the consumer or authorized representative to take steps to generate a record, such as providing a signature or recording verbal confirmation, and must include, at a minimum, the following information:
- A description of the scope, purpose, and duration of the consent provided by the consumer or their authorized representative.
- The date on which consent was given.
- The name of the consumer or their authorized representative.
- The name of the agent to whom consent is granted.
- A process through which the consumer or authorized representative can revoke consent.
Form 2: New eligibility application confirmation requirements:
Agents must obtain and document that eligibility application information has been reviewed and confirmed by the consumer before submitting the coverage application through federally facilitated exchanges and state exchanges on the federal platform.
This consumer consent for application accuracy requires the consumer or authorized representative to take steps to generate a record (e.g., providing a signature or recording verbal confirmation) that must include, at a minimum, the following information:
- The date on which the application information was reviewed.
- The name of the consumer or their authorized representative.
- An explanation of the certifications at the end of the eligibility application.
- The name of the assisting agent.
Important: Documentation for these two new requirements must be retained for a minimum of 10 years and be available upon request in response to monitoring, auditing, and compliance activities.
These new requirements have been formed under the Patient Protection and Affordable Care Act: Notice of Benefits and Payment Parameters for 2024 by the HHS and will help with:
- Resolving consumer complaints related to incorrect information in their eligibility applications or unauthorized enrollments.
- Resolving disputes between agents and consumers or between multiple registering entities.
Procedures:
CMS – Form 1 and its variants by referral (override) & Form 2
Form 1: consent with its 4 variants: F1E or FB1FE or MF1E or OF1E, includes the NPN related to the referral (override) in those cases that are required.
Form 2: the confirmation with one variant, F2E (English).
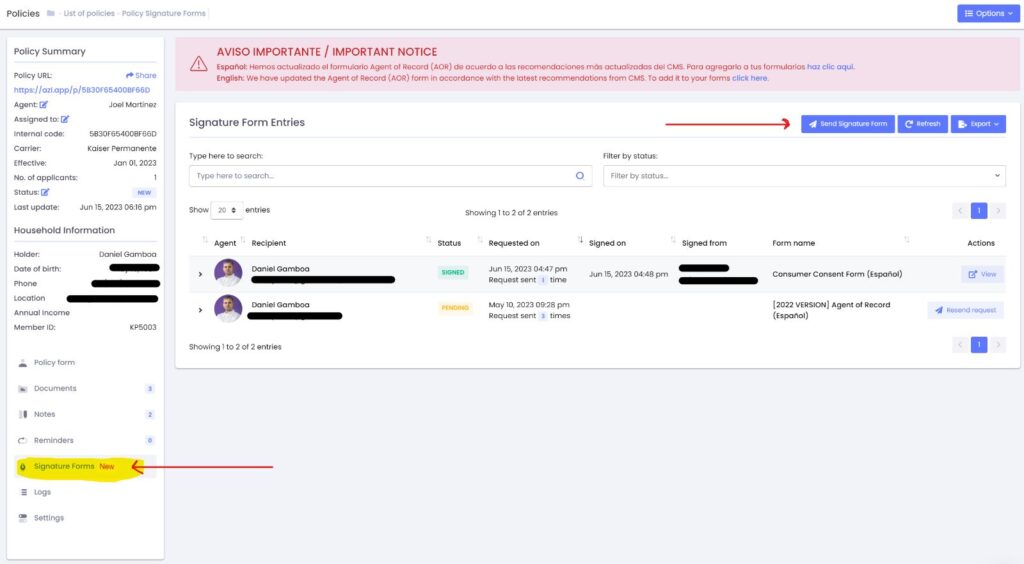
Procedure: a Form 1 must be selected to which a Form 2 will be added. In total there will be 2 forms, F1 + F2, for the signature of the client/principal.
Code Description to facilitate your search:
Forms to be used when referral is not required, both F1 & F2 must be selected in English or Spanish, in total two forms to be signed by the client/principal:
- F1E – Consumer Consent Form (1 English)
- F2E – Consumer Eligibility Application Confirmation Form (2 English)
F1 forms to be used when it is required to refer to which F2E or F2S must be added, depending on whether it is English or Spanish, in total two forms to be signed by the client/principal:
Considerations for the Apizeal platform:
Everyone
must see it at any time whether they have extended structure or not. Important:
– For extended structures, all forms were added in INACTIVE status by default. In order to send them they must review them, verify that they look good and mark
them as active. The reason for this is because before they can send them they must at least see them first and if they see everything ok then activate them.
– If someone has yet to see the forms on their portals, please contact us via chat so we can add them as we did last time, especially since there are many new
extended structures that perhaps did not enter the previous monitoring process.
Regarding phone numbers: It is not possible to use your phone numbers to send messages; technically, it is impossible.
Sending messages through applications must compulsorily contract a number with the platform they want to use. And they must notify their clients that they will now receive communications through that number.
Each person has their unique number that is not shared.
You don’t have to worry about messages from other agents being sent from the numbers you reserve.
Sending Forms via text messaging (Signature Forms, ninth link):
To send either of the two forms via text messaging, you must first create a messaging account. Follow these steps:
- In the left sidebar menu, click on the “SMS Marketing” option.
- Add a credit or debit card to your virtual wallet by clicking on the “ADD CREDIT/DEBIT CARD” button.
- Then click on the “CREATE SMS ACCOUNT” button and follow the steps instructed by the system.
After creating the messaging account:
You must verify your new Toll-Free number in the USA. Please click on the link to initiate the verification process, in the ninth link: Apizeal | Health and Life Insurance Management System
If you have any questions, please contact Apizeal through their accounts using the chat support.